What Is Female Sterilization?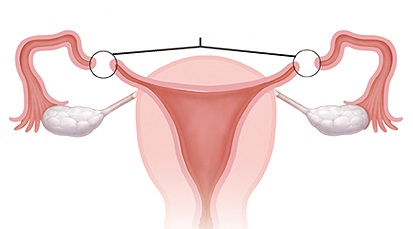
One of the most effective methods but carries a small risk of failure:
Fertility does not return because sterilization generally cannot be stopped or reversed. The procedure is intended to be permanent. Reversal surgery is difficult, expensive, and not available in most areas. When performed, reversal surgery often does not lead to pregnancy
Protection against sexually transmitted infections (STIs): None
Side Effects
None.
Known Health Benefits
Helps protect against:
May help protect against:
Imporoove:
Known Health Risks
Uncommon to extremely rare:
Complications
Uncommon to extremely rare:
The risk of complications with local anesthesia is significantly lower than with general anesthesia. Complications can be kept to a minimum if appropriate techniques are used and if the procedure is performed in an appropriate setting.
Safe for All Women
With proper counseling and informed consent, any woman can have female sterilization safely, including women who:
In some of these situations, especially careful counseling is important to make sure the woman will not regret her decision.
Women can have female sterilization:
Female sterilization:
Problems Reported as Complications::
Contact your doctor if you have any of the problems listed above.
1. Will sterilization change a woman’s monthly bleeding or make monthly bleeding stop?
No. Most research finds no major changes in bleeding patterns after female sterilization. If a woman was using a hormonal method or IUD before sterilization, her bleeding pattern will return to the way it was before she used these methods. For example, women switching from combined oral contraceptives to female sterilization may notice heavier bleeding as their monthly bleeding returns to usual patterns. Note, however, that a woman’s monthly bleeding usually becomes less regular as she approaches menopause.
2. Will sterilization make a woman lose her sexual desire? Will it make her fat?
No. After sterilization a woman will look and feel the same as before. She can have sex the same as before. She may find that she enjoys sex more because she does not have to worry about getting pregnant. She will not gain weight because of the sterilization procedure.
3. Should sterilization be offered only to women who have had a certain number of children, who have reached a certain age, or who are married?
No. There is no justification for denying sterilization to a woman just because of her age, the number of her living children, or her marital status. Health care providers must not impose rigid rules about age, number of children, age of last child, or marital status. Each woman must be allowed to decide for herself whether or not she will want more children and whether or not to have sterilization.
4. Is it not easier for the woman and the health care provider to use general anesthesia? Why use local anesthesia?
Local anesthesia is safer. General anesthesia is more risky than the sterilization procedure itself. Correct use of local anesthesia removes the single greatest source of risk in female sterilization procedures—general anesthesia. Also, after general anesthesia, women usually feel nauseous. This does not happen as often after local anesthesia. When using local anesthesia with sedation, however, providers must take care not to overdose the woman with the sedative. They also must handle the woman gently and talk with her throughout the procedure. This helps her to stay calm. With many clients, sedatives can be avoided, especially with good counseling and a skilled provider.
5. Does a woman who has had a sterilization procedure ever have to worry about getting pregnant again?
Generally, no. Female sterilization is very effective at preventing pregnancy and is intended to be permanent. It is not 100% effective, however. Women who have been sterilized have a slight risk of becoming pregnant: About 5 of every 1,000 women become pregnant within a year after the procedure. The small risk of pregnancy remains beyond the first year and until the woman reaches menopause.
6. Pregnancy after female sterilization is rare, but why does it happen at all?
Most often it is because the woman was already pregnant at the time of sterilization. In some cases an opening in the fallopian tube develops. Pregnancy also can occur if the provider makes a cut in the wrong place instead of the fallopian tubes.
7. Can sterilization be reversed if the woman decides she wants another child?
Generally, no. Sterilization is intended to be permanent. People who may want more children should choose a different family planning method. Surgery to reverse sterilization is possible for only some women—those who have enough fallopian tube left. Even among these women, reversal often does not lead to pregnancy. The procedure is difficult and expensive, and providers who are able to perform such surgery are hard to find. When pregnancy does occur after reversal, the risk that the pregnancy will be ectopic is greater than usual. Thus, sterilization should be considered irreversible.
8. Is it better for the woman to have female sterilization or the man to have a vasectomy?
Each couple must decide for themselves which method is best for them. Both are very effective, safe, permanent methods for couples who know that they will not want more children. Ideally, a couple should consider both methods. If both are acceptable to the couple, vasectomy would be preferable because it is simpler, safer, easier, and less expensive than female sterilization.
9. Will the female sterilization procedure hurt?
Yes, a little. Women receive local anesthetic to stop pain, and, except in special cases, they remain awake. A woman can feel the health care provider moving her uterus and fallopian tubes. This can be uncomfortable. If a trained anesthetist or anesthesiologist and suitable equipment are available, general anesthesia may be chosen for women who are very frightened of pain. A woman may feel sore and weak for several days or even a few weeks after surgery, but she will soon regain her strength.
10. How can health care providers help a woman decide about female sterilization?
Provide clear, balanced information about female sterilization and other family planning methods, and help a woman think through her decision fully. Thoroughly discuss her feelings about having children and ending her fertility. For example, a provider can help a woman think how she would feel about possible life changes such as a change of partner or a child’s death.
11. Does female sterilization increase the risk of ectopic pregnancy?
No. On the contrary, female sterilization greatly reduces the risk of ectopic pregnancy. Ectopic pregnancies are very rare among women who have had a sterilization procedure. The rate of ectopic pregnancy among women after female sterilization is 6 per 10,000 women per year. The rate of ectopic pregnancy among women in the United States using no contraceptive method is 65 per 10,000 women per year. On the rare occasions that sterilization fails and pregnancy occurs, 33 of every 100 (1 of every 3) of these pregnancies are ectopic. Thus, most pregnancies after sterilization failure are not ectopic. Still, ectopic pregnancy can be life-threatening, so a provider should be aware that ectopic pregnancy is possible if sterilization fails.
12. Where can female sterilization be performed?
If no pre-existing medical conditions require special arrangements:
13. What are transcervical methods of sterilization?
Transcervical methods involve new ways of reaching the fallopian tubes, through the vagina and uterus. A microcoil, Essure, is already available in some countries. Essure is a spring-like device that a specifically trained clinician using a viewing instrument (hysteroscope) inserts through the vagina into the uterus and then into each fallopian tube. Over the 3 months following the procedure, scar tissue grows into the device. The scar tissue permanently plugs the fallopian tubes so that sperm cannot pass through to fertilize an egg. Essure is unlikely to be introduced in low-resource settings soon, however, because of the high cost and complexity of the viewing instrument required for insertion.
For a family planning consultation:
What Is Vasectomy?
One of the most effective methods but carries a small risk of failure:
Fertility does not return because vasectomy generally cannot be stopped or reversed. The procedure is intended to be permanent. Reversal surgery is difficult, expensive, and not available in most areas. When performed, reversal surgery often does not lead to pregnancy.
Protection against sexually transmitted infections (STIs): None
Side Effects, Known Health Benefits and Health Risks
None
Complications
Uncommon to rare:
Uncommon to very rare:
Rare:
Safe for All Men
With proper counseling and informed consent, any man can have a vasectomy safely, including men who:
In some of these situations, especially careful counseling is important to make sure the man will not regret his decision.
Men can have a vasectomy:
Vasectomy:
Problems Reported as Complications::
Contact your doctor if you have any of the problems listed above.
1. Will vasectomy make a man lose his sexual ability? Will it make him weak or fat?
No. After vasectomy, a man will look and feel the same as before. He can have sex the same as before. His erections will be as hard and last as long as before, and ejaculations of semen will be the same. He can work as hard as before, and he will not gain weight because of the vasectomy.
2. Will there be any long-lasting pain from vasectomy?
Some men report having chronic pain or discomfort in the scrotum or testicles that can last from 1 to 5 years or more after a vasectomy. In the largest studies, involving several thousand men, less than 1% reported pain in the scrotum or testicles that had to be treated with surgery. In smaller studies, of about 200 men, as many as 6% reported severe pain in the scrotum or testicles more than 3 years after the vasectomy. In a similar group of men who did not have vasectomies, however, 2% reported similar pain. Few men with severe pain say that they regret having the vasectomy. The cause of the pain is unknown. It may result from pressure caused by the build-up of sperm that has leaked from an improperly sealed or tied vas deferens, or from nerve damage.
Treatment includes elevating the scrotum and taking pain relievers. An anesthetic can be injected into the spermatic cord to numb the nerves to the testicles. Some providers report that surgery to remove the painful site or reversing the vasectomy relieves the pain. Severe, long-lasting pain following vasectomy is uncommon, but all men considering a vasectomy should be told about this risk.
3. Does a man need to use another contraceptive method after a vasectomy?
Yes, for the first 3 months. If his partner has been using a contraceptive method, she can continue to use it during this time. Not using another method for the first 3 months is the main cause of pregnancies among couples relying on vasectomy
4. Is it possible to check if a vasectomy is working?
Yes. A provider can examine a semen sample under a microscope to see if it still contains sperm. If the provider sees no moving (motile) sperm, the vasectomy is working. A semen examination is recommended at any time after 3 months following the procedure, but is not essential. If there is less than one nonmotile sperm per 10 high-power fields (less than 100,000 sperm per milliliter) in the fresh sample, then the man can rely on his vasectomy and stop using a backup method for contraception. If his semen contains more moving sperm, the man should continue to use a backup method and return to the clinic monthly for a semen analysis. If his semen continues to have moving sperm, he may need to have a repeat vasectomy.
5. What if a man’s partner gets pregnant?
Every man having a vasectomy should know that vasectomies sometimes fail and his partner could become pregnant as a result. He should not make the assumption that his partner was unfaithful if she becomes pregnant. If a man’s partner becomes pregnant during the first 3 months after his vasectomy, remind the man that for the first 3 months they needed to use another contraceptive method.
If possible, offer a semen analysis and, if sperm are found, a repeat vasectomy.
6. Will the vasectomy stop working after a time?
Generally, no. Vasectomy is intended to be permanent. In rare cases, however, the tubes that carry sperm grow back together and the man will require a repeat vasectomy.
7. Can a man have his vasectomy reversed if he decides that he wants another child?
Generally, no. Vasectomy is intended to be permanent. People who may want more children should choose a different family planning method. Surgery to reverse vasectomy is possible for only some men and reversal often does not lead to pregnancy. The procedure is difficult and expensive, and providers who are able to perform such surgery are hard to find. Thus, vasectomy should be considered irreversible.
8. Is it better for the man to have a vasectomy or for the woman to have female sterilization?
Each couple must decide for themselves which method is best for them. Both are very effective, safe, permanent methods for couples who know that they will not want more children. Ideally, a couple should consider both methods. If both are acceptable to the couple, vasectomy would be preferable because it is simpler, safer, easier, and less expensive than female sterilization.
9. How can health care providers help a man decide about vasectomy?
Provide clear, balanced information about vasectomy and other family planning methods, and help a man think through his decision fully. Thoroughly discuss his feelings about having children and ending his fertility. For example, a provider can help a man think how he would feel about possible life changes such as a change of partner or a child’s death. Review The 6 Points of Informed Consent to be sure the man understands the vasectomy procedure.
10. Should vasectomy be offered only to men who have reached a certain age or have a certain number of children?
No. There is no justification for denying vasectomy to a man just because of his age, the number of his living children, or his marital status. Health care providers must not impose rigid rules about age, number of children, age of last child, or marital status. Each man must be allowed to decide for himself whether or not he will want more children and whether or not to have vasectomy.
11. Does vasectomy increase a man’s risk of cancer or heart disease later in life?
No. Evidence from large, well-designed studies shows that vasectomy does not increase risks of cancer of the testicles (testicular cancer) or cancer of the prostate (prostate cancer) or heart disease.
12. Can a man who has a vasectomy transmit or become infected with sexually transmitted infections (STIs), including HIV?
Yes. Vasectomies do not protect against STIs, including HIV. All men at risk of STIs, including HIV, whether or not they have had vasectomies, need to use condoms to protect themselves and their partners from infection.
13. Where can vasectomies be performed?
If no pre-existing medical conditions require special arrangements, vasectomy can be performed in almost any health facility, including health care centers, family planning clinics, and the treatment rooms of private doctors. Where other vasectomy services are not available, mobile teams can perform vasectomies and any follow-up examinations in basic health facilities and specially equipped vehicles, so long as basic medications, supplies, instruments, and equipment can be made available.
For a family planning consultation: